 |
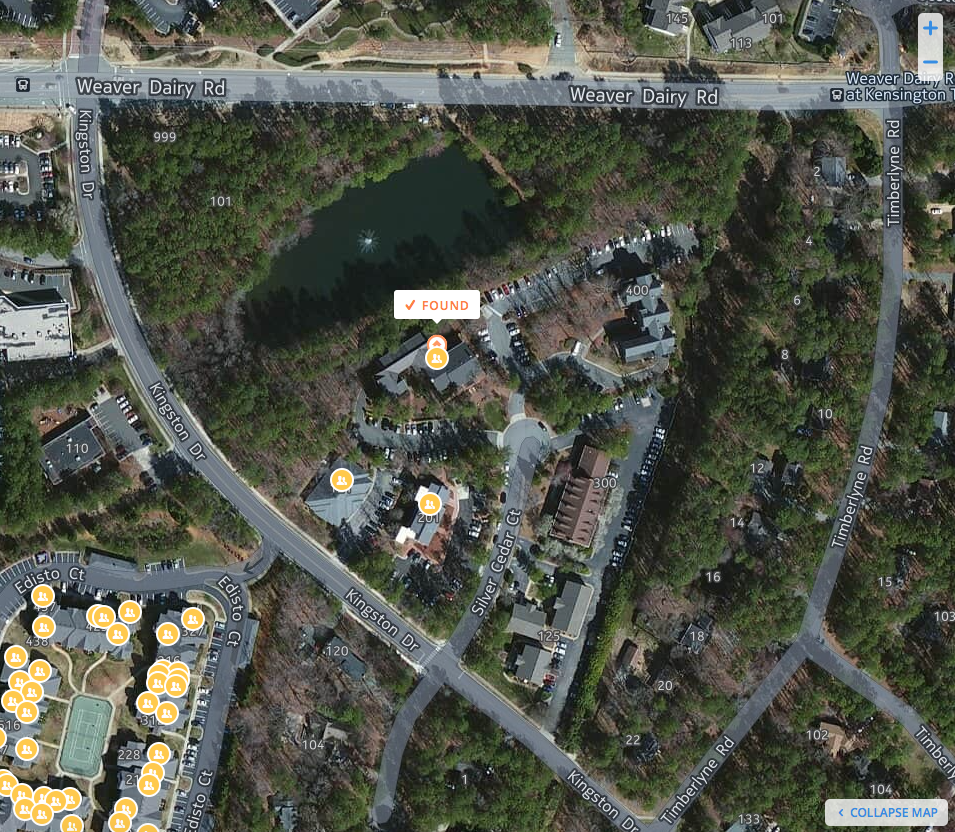
| Satellite view of the American Board of Pediatrics' 2.8-acre Pond |
Surely, US pediatricians need a 2.8 acre pond. Where else would they be able to sit and contemplate their past careers as academics as the sun sets slowly over the horizon? Everyone knows that when properly maintained, ponds provide a peaceful venue for a leisurely stroll or for the opportunity to toss a hook and bobber in search of a bluegill or large-mouth bass. No doubt these activities are critical pediatric health care quality and safety skills. Thanks to the leadership and "medical professionalism" portrayed by the ABP leadership over the past 30 years or so, all US pediatricians can feel proud to know that every bit of their $1200 "continuous MOC" fee is going to the support of this worthy landmark.
Surely pediatricians worldwide know about the pond they purchased, don't they?
Perhaps not.
Ponds, you see, don't typically make the internet websites of the American Board of Medical Specialties member boards or IRS Form 990 tax forms (except as "land and buildings"). Few would think of lands and buildings as including a pond, but for the American Board of Pediatrics, it does. In fact, their pond (picture) rests on a consortium of properties adjacent to 111 Silver Cedar Ct, Chapel Hill, NC that span over 9.3 acres and comprises two separate buildings (201 Silver Cedar Ct is also owned by the ABP). Unfortunately, it's hard to imagine how a pond adds to the safety or quality of pediatric care in the United States. Instead, we can only surmise that a pond is an important asset to the American Board of Pediatrics because it improves their property value and provides important tax revenues and political influence to the state of North Carolina and beyond.
And who better to pay for that pond and annual taxes than unsuspecting US pediatricians increasingly forced to comply with Maintenance of Certification?
No one was supposed to know that the first recorded deed of these properties coincided in time with the creation of Maintenance of Certification, 1986, according to North Carolina real estate records. No one was supposed to know that as President and Advisor to the American Board of Pediatrics, James A. Stockman, III, MD, earned $1,307,415 in Fiscal year 2012 before his retirement package of another $2.4 million kicked in the next year, either.
And let's not forget the many cars that pediatric diplomates helped Dr. Stockman purchase during his tenure at the ABP.
Here are Dr. Stockman's own words, published in Pediatric Annals:
Dr. Shulman: If you had not chosen medicine, which field would you have chosen?Life beyond academe indeed.
Dr. Stockman: I’d be a car salesman.
Dr. Shulman: I suppose that’s not a surprise. You are quite the collector of classic cars. Your wife once told me that during a 5-year period in Chicago you bought and sold 40 or 50 separate autos. And that was before eBay!
Dr. Stockman: Yes, my collection is very diverse. Among them are a ’56 Cadillac, a Sting Ray, a Triumph, and a twin turbo engine Porsche 911. I love driving them on all the country back roads here in North Carolina. There is life beyond academe!…
Especially when one considers that Maintenance of Certification (MOC) was Stockman's "most far-reaching achievement" of his 20-year career with the American Board of Pediatrics (according to the well-funded Illinois-based American Academy of Pediatrics that has an extensive lobbying presence on Capitol Hill).
-Wes