I'll be restoring the creative juices. I'll be back Sunday or Monday. Have a nice weekend.
-Wes
Thursday, July 31, 2008
More Light on the Pacemaker/CT Scanner Interaction
St. Jude Medical came forth with a "Dear Doctor" letter (pdf) today regarding their findings regarding pacemaker and CT scanner interactions which represents the most specific recommendations with CT scanners and their devices to date:
Medtronic's statement regarding the same issue is included here (pdf).
I cannot recall ever seeing an interaction like the one they're describing, but the implications are that we'll have to be more cautious as CT scanners become more powerful, especially as patients have chest CT's that might scan the pacemaker implant sight. For the great majority of patients, I just do not see this as a "biggie" for patient care. Anyone else with thoughts?
-Wes
Testing has shown that for devices which incorporate an accelerometor for rate responsive activity-based pacing, if the activity sensor is programmed "on" while continuous diagnostic X-ray exposure (e.g. CT scanning) is performed, if the beam of energy is directly over the implanted device, there may be a temporary increase in pacing rate during the exposure. The pacing rate will return to baseline pacing after the X-ray exposure is terminated. If increased rates occur, the pacing rate will be limited to the programmable Maximum Sensor Rate which is generally determined by the patient's physician as the safe maximum rate to be achieved during exercise. To prevent any potential transient rate increase, the clinician may want to consider programming the rate responsive sensor to Passive or OFF, if appropriate, prior to the X-ray procedure and then reprogram the parameter as desired after the diagnostic imaging is completed.Read the rest for the details.
Medtronic's statement regarding the same issue is included here (pdf).
I cannot recall ever seeing an interaction like the one they're describing, but the implications are that we'll have to be more cautious as CT scanners become more powerful, especially as patients have chest CT's that might scan the pacemaker implant sight. For the great majority of patients, I just do not see this as a "biggie" for patient care. Anyone else with thoughts?
-Wes
Wednesday, July 30, 2008
EKG's and ADHD: Common Sense Prevails
I'm so glad 'dem der pediatricians set us here cardiologists straight.
Dang, I had no idear there was so many of 'dem der corrections to the original announcement about the need for EKG's before administering ADHD drugs.
Nice to know some common sense could prevail...
-Wes
Dang, I had no idear there was so many of 'dem der corrections to the original announcement about the need for EKG's before administering ADHD drugs.
Nice to know some common sense could prevail...
-Wes
Determining Cause and Effect
I wouldn't want the FDA's job.
Today, the Chicago Tribune reported that of the 93 deaths from "tainted" heparin, that analphylaxis (a sudden allergic reaction with associated drop in blood pressure) was identified in 10 of the 93. Of these 10, 3 patients were conclusively found to have the "oversulfated chondroitin sulfate" contaminant in certain vials:
The FDA should be commended on their efforts to cull through a vast sea of medical information to attempt to determine the cause of death in the individuals affected and working so quickly to determine a cause of the contaminant. To me, finding three deaths in a sea of 90 deaths that were definitively determined to be related to the contaminant is like finding a needle in a haystack. Perhaps more importantly, by issuing their summative findings of the evalutation of the deaths, they shed light on the difficulty of monitoring and investigating drug reactions from community-based reporting.
-Wes
Today, the Chicago Tribune reported that of the 93 deaths from "tainted" heparin, that analphylaxis (a sudden allergic reaction with associated drop in blood pressure) was identified in 10 of the 93. Of these 10, 3 patients were conclusively found to have the "oversulfated chondroitin sulfate" contaminant in certain vials:
Of 10 reports of death from severe shock known as anaphylaxis or hypotension, three of those could be traced to lot numbers of Baxter products that tested positive for an animallike substance known as oversulfated chondroitin sulfate. Heparin lot numbers were not known for the other seven deaths from anaphylaxis or hypotension, so the FDA could not determine whether those 7 patients received heparin contaminated with the substance.But what I found interesting were the number of deaths NOT found related to the contaminant. Of the remaining 83 deaths reported:
- 45 didn't have enough data submitted to be able to determine a cause of death
- 25 were causes unrelated to heparin, like kidney failure, pneumonia, and sepsis
- 13 were related to bleeding, a known side effect of heparin
The FDA should be commended on their efforts to cull through a vast sea of medical information to attempt to determine the cause of death in the individuals affected and working so quickly to determine a cause of the contaminant. To me, finding three deaths in a sea of 90 deaths that were definitively determined to be related to the contaminant is like finding a needle in a haystack. Perhaps more importantly, by issuing their summative findings of the evalutation of the deaths, they shed light on the difficulty of monitoring and investigating drug reactions from community-based reporting.
-Wes
Tuesday, July 29, 2008
Taking the Leap: Why Medicine?
Edwin Leap, MD hosts Grand Rounds this week:
Because.
-Wes
"... my theme this week is ‘Why do we do it?’ That is, medicine being what it is, many providers (nurses, physicians, PA’s, NP’s, etc) are dissatisfied and frustrated. So why is it that all of these good people keep coming back? Why do docs like me return to the packed, over-burdened, understaffed emergency department, day after day, year after year? Why do surgeons operate at all hours on the injured and dying, aging too quickly and leaving their families at home? Why do family doctors care for so many complicated and ungrateful individuals…at a financial loss? Why do students sacrifice so much of their lives to become physicians? Why do nurses endure the hours and patient ratios, the annoying physicians and the pesky families in order to care for the sick? Why do we do it?"Why?
Because.
-Wes
EKG Du Jour - #10
Ah, it's been a while since I've pulled an EKG from the EKG Hall of Fame series, so here's the tenth installment for your enjoyment:*
A 28 year old man presents to your office with an implantable cardiac defibrillator (ICD) in place. He shows you his EKG, shown here:

You are asked for a second opinion to see if he really needs his ICD. He has no reports from the other hospital with him.
What is the differential diagnoses offered by this EKG, and of those, given his age and EKG findings, what might be the most likely diagnosis?
-Wes
* Prior "EKGs Du Jour" can be reviewed by typing "Du Jour" in the search box on the right side bar of this blog.
A 28 year old man presents to your office with an implantable cardiac defibrillator (ICD) in place. He shows you his EKG, shown here:

Click image to enlarge
You are asked for a second opinion to see if he really needs his ICD. He has no reports from the other hospital with him.
What is the differential diagnoses offered by this EKG, and of those, given his age and EKG findings, what might be the most likely diagnosis?
-Wes
* Prior "EKGs Du Jour" can be reviewed by typing "Du Jour" in the search box on the right side bar of this blog.
Quote of the Day
 Today, San Francisco's city board of supervisors will vote on whether to bar cigarette sales at pharmacies and retail stores with in-store clinics that treat common ailments such as sore throats and sinus infections as of October 1. Opponents of the tobacco ban believe stores will get out of the clinic business if they are forced to choose between providing health care and selling cigarettes:
Today, San Francisco's city board of supervisors will vote on whether to bar cigarette sales at pharmacies and retail stores with in-store clinics that treat common ailments such as sore throats and sinus infections as of October 1. Opponents of the tobacco ban believe stores will get out of the clinic business if they are forced to choose between providing health care and selling cigarettes:"We do not understand how forcing retailers to choose between having an in-store clinic and selling tobacco products serves the broader goal of providing consumers with easier access to high-quality, affordable health care"Perhaps, Ms. Hansen-Turton, it's because healthcare is about commitment to real health, not just convenience and profit. Frankly, I can't think of a better way to promote sore throats and sinus infections than to sell cigarettes, too.
- Tine Hansen-Turton
Executive Director of the Convenient Care Association
-Wes
Image reference.
Monday, July 28, 2008
Thoughts on the Canadian Health Care System
It seems that dogs can get hips before people:
-Wes
From that beginning, in 1958 the clinic expanded to Bank Street at Alta Vista. In 1986, it built a modern new 10,400-square-foot facility further out Bank Street. In 2001, a 13,000-square-foot wing was added. It now has 22 vets, 40 animal health technicians, and about 85 support staff. Specialists include internal medicine, cardiology, surgery, oncology and dentistry.Ah, the power of cash.
It has its own high-tech scanners, and can do hip and joint replacements in a fraction of the waiting time people are forced to endure. It is a major supporter of most animal welfare campaigns.
-Wes
Making 'Em Look Good
It’s the beginning of the academic medical school year, and a new flock of energetic medical students has arrived. It is evident as they eagerly call the attending to “notify” them of a sick case that was “coming to the ward” having never seen the patient.
It was no biggie, this time. Things were handled. But it was clear during the late-night phone conversation that the medical student hadn’t seen the patient, wasn’t aware of the entire medical history, and was sent as the “messenger.”
Well, we don’t shoot the messenger.
But there’s also an important principle that should be followed when communicating with different members of the medical team involved in a patient’s care:
Make ‘em look good.
If you are a medical student, make your resident look good on rounds. Know the history, medications, lab results, and the patient’s chief complaint that day. If you do, he’ll make sure you look good.
If you’re a resident, make your fellow look good on rounds. Teach the students. Check the patient yourself if needed. Give the fellow the pertinent items to be addressed that day, and make sure they happen. If you do, your fellow will make you look good.
If you’re a fellow, make your attending look good on rounds. Guide the resident. Come prepared, having communicated with the team, understand the next plan of action, and implement it. If you do, your attending will make you look good.
If you’re an attending, make sure the nurse looks good. Point out the good things he or she did overnight, guide them on the items that need attention, and listen to their concerns. If you do, your nurse will make you look good.
If you’re a nurse, make sure the patient looks good. Respond to their calls, check the medications not once but twice, ask why the dinner tray arrived late, and help brush the patient's hair and teeth. If you do, the patient will make sure the whole hospital looks good.
Simple, effective.
That’s the way it works.
Best of luck to all of you.
-Wes
It was no biggie, this time. Things were handled. But it was clear during the late-night phone conversation that the medical student hadn’t seen the patient, wasn’t aware of the entire medical history, and was sent as the “messenger.”
Well, we don’t shoot the messenger.
But there’s also an important principle that should be followed when communicating with different members of the medical team involved in a patient’s care:
Make ‘em look good.
If you are a medical student, make your resident look good on rounds. Know the history, medications, lab results, and the patient’s chief complaint that day. If you do, he’ll make sure you look good.
If you’re a resident, make your fellow look good on rounds. Teach the students. Check the patient yourself if needed. Give the fellow the pertinent items to be addressed that day, and make sure they happen. If you do, your fellow will make you look good.
If you’re a fellow, make your attending look good on rounds. Guide the resident. Come prepared, having communicated with the team, understand the next plan of action, and implement it. If you do, your attending will make you look good.
If you’re an attending, make sure the nurse looks good. Point out the good things he or she did overnight, guide them on the items that need attention, and listen to their concerns. If you do, your nurse will make you look good.
If you’re a nurse, make sure the patient looks good. Respond to their calls, check the medications not once but twice, ask why the dinner tray arrived late, and help brush the patient's hair and teeth. If you do, the patient will make sure the whole hospital looks good.
Simple, effective.
That’s the way it works.
Best of luck to all of you.
-Wes
Like Moths Drawn to a Light

Once again, Pay for Performance measures have been demonstrated to be a miserable bureaucratic failure.
But what's the bureaucrats' response? Why, PAY THEM MORE and MAKE MORE MEASURES to make it work, of course!
Rosenthal cautioned that studies finding little quality impact so far "have nothing to do with overturning the theory of pay-for-performance. It can be explained by the way in which these programs have been implemented, and at the top of the list is that the size of the bonus is too small."Don't they get it? THIS DOESN'T WORK! Worse yet, people can get RICH scheming this system: just build a little algorithm to assure everyone gets a test each time they're seen, (performed, of course, under the guise of a "quality initiative") whether they need it or not, and voila' - you're rich! You can name a TON of ways to game the system because each of these "measures" turns the intent of "quality" into a PROFIT motive for doctors and hospitals.*
Maximum quality incentives average 9% of plan payments, according to a Nov. 2, 2006, New England Journal of Medicine study by Rosenthal, but most physicians average less than a 5% bonus. By contrast, under a British P4P plan that was rolled out in 2004, physicians can more than double their income by achieving high scores on 149 quality indicators.
When it comes to pay and the inevitable declining revenues in the Medicare National Bank, doctors (and hospitals) are like moths: they're drawn to the brightest light with this month's payment rationing scheme. And here's the thing...
...the brighter the light, the more moths will flock there.
-Wes
* Well, not really. Actually Medicare withholds a portion of payments to doctors and hospitals first, and only after completing 85% or more of the "quality measures" will they ante up the full payment amount. (It's like training a dog: "Sit, Fido, sit. Stay. Staaayyy. Good, dog! Here's your treat!")
Image reference.
Sunday, July 27, 2008
Pinching Childhood Brain Cancer
 Our infamous Dr. Rob of Musings of a Distractible Mind has been working tirelessly with Zippy, the lovable red lobster, to raise awareness and funds to support childhood brain cancer research over at FunWithZippy.com. He asked if we'd help support the effort and host the official "Fun With Zippy" t-shirt on our medical t-shirt site MedTees.com, for which we were only too happy to help out.
Our infamous Dr. Rob of Musings of a Distractible Mind has been working tirelessly with Zippy, the lovable red lobster, to raise awareness and funds to support childhood brain cancer research over at FunWithZippy.com. He asked if we'd help support the effort and host the official "Fun With Zippy" t-shirt on our medical t-shirt site MedTees.com, for which we were only too happy to help out.All proceeds from the sales of these shirts, button, aprons, mouse-pads, stickers and the like with Zippy's logo will support childhood brain cancer research.
Why not help some kids out today and get your very own shirt? After all, you never know where Zippy will show up next.
-Wes
The Power of Marketing Drugs for Kids

...it's especially evident in our new, burgeoning pharmaceutical market, our children:
Madeira Therapeutics, based in Leawood, Kan., is formulating a liquid statin for children that will be sold in either grape, cherry or bubblegum flavor, according to the company’s chief executive, Peter R. Joiner.This need is further supported, of course, by powerful marketing data supplied by the monstrously profitable prescription services themselves: Medco Health Solutions, Express Scripts, and Verispan:
Madeira became interested in the drug to treat children with a genetic cholesterol condition, familial hypercholesterolemia, which strikes 1 in 500 children regardless of their diet. The recent American Academy of Pediatrics statement adds to the potential market, according to Mr. Joiner.
Express Scripts and Medco developed estimates of how many children might be taking such drugs by extrapolating their data — involving a total of more than four million children — across the broader population.And therefore, because the rates have climbed, it must be okay, right?
The companies use different assumptions to reach their estimates, but the data suggests that at least several hundred thousand children are on various obesity-related medications.
The greatest increase occurred in drugs for Type 2 diabetes, with Medco’s data showing a 151 percent jump from 2001 to 2007.
Medco’s data, released in May, showed that use of drugs to treat acid reflux problems in children, often aggravated by obesity, increased 137 percent over seven years. Its analysis also showed an 18 percent increase in drugs to treat high blood pressure and a 12 percent increase in cholesterol-lowering medications during the seven-year period.
Express Scripts found a 15 percent increase over three years in drugs to treat cholesterol and other fats in the blood, a category that is primarily statins.
“We were amazed at how quickly the rates of drugs used have climbed,” said Dr. Donna R. Halloran, an assistant professor at St. Louis University who worked on the Express Scripts analysis, presented at a meeting of the American Public Health Association in November.
Verispan data recorded a 13 percent increase in high blood pressure prescriptions in the under 19 age group from 2005 to 2007. Its numbers show, however, a less than 1 percent increase during the period in cholesterol-lowering drugs in children.
The suspect nature of these culled data draw into question the message we want to feed (pun intended) our children and families, and pushes public health experts (and even our professional societies) to waddle toward the path of least resistance when it comes to caring for our children.
The issue of childhood obesity is a complicated one, fraught with many challenges. The influence of the fast-food industry, internet gaming industry, drops in funding to support school-based physical education programs, and the complicated socioeconomic challenges of fragmented families, have all coalesced to create the perfect storm of influences to promote weight gain in our children. These problems, it seems, have become insurmountable.
Better to just give 'em a pill.
-Wes
Image reference.
Friday, July 25, 2008
Fat Chance That Trans Fat Ban Will Help
Let me see if I have this right:
No wonder patients are confused.
-Wes
"A Low-Carbohydrate, Ketogenic Diet versus a Low-Fat Diet To Treat Obesity and Hyperlipidemia" showed low-carbohydrate, ketogenic (high fat) diets were superior to a low-fat diets for weight loss and lipid management.So given all of this prospective, randomized data, why the heck is California so proud to be banning trans fats? Trans fats exist in many, many foods besides baking oils. Meats, butter, and milk all have trans fats. Given the available data above and the efficancy of LOW CARDBOHYDRATE diets to improve weight and lipid panels, might they be targeting the wrong thing?
"A randomized controlled trial of a moderate-fat, low-energy diet compared with a low fat, low-energy diet for weight loss in overweight adults" demonstrated the moderate fat diet helped dieters lose weight faster than low-fat diets.
In a "Comparison of the Atkins, Zone, Ornish, and LEARN Diets for Change in Weight and Related Risk Factors Among Overweight Premenopausal Women," the Atkins diet, with its high fat, won hands down at weight loss and lipid improvement in women.
And now, in the DIRECT Trial testing "Weight Loss with a Low-Carbohydrate, Mediterranean, or Low-Fat Diet," we find that low carbohydrate (moderate fat) or Mediterranean diets are superior to low-fat diets at weight loss and lipid management.
No wonder patients are confused.
-Wes
Double Trouble: Nurses Gone Wild
It's bad anough having one nurse stealing drugs, but it's even worse when there's two co-workers colluding together:
-Wes
Det. Scharschmidt says O'Grady knew Hughs' work schedule and the two coordinated the times when O'Grady would go to an area pharmacy to pass a prescription. When the pharmacist would call the medical office to check on the prescription, Hughs would answer the phone, assuring the pharmacist that the prescription was good.Scary scenario, indeed.
Investigators say Hughs had as many as 30 different aliases she used on the prescriptions to get drugs like Oxycontin, Percocet, Hydrocodone, and Alprazolam.
Parma Heights Police say many of those drugs were then sold on the street.
"One of the females, O'Grady, had had an Oxycontin addiction so some of this was for personal consumption," Said Det. Scharschmidt, "but for the most part they were being sold on the streets and turned into a financial gain for the two of them."
Police estimate that both women obtained 20,000 pills over the course of three or four years, making as much as $200,000.
-Wes
I Didn't Practice Evidence-Based Medicine Today
 He was 70 with critical aortic stenosis and ejection fraction of 10%, coronary artery disease and history of 5-vessel bypass in 2001, a history of Stage D colon cancer with lung mets resected 18 months ago, obesity, diabetes mellitus, chronic renal insufficiency and was recently extubated after a failed aortic valvuloplasty. He later developed a wide complex tachycardia at 150 beats per minute for which I was asked to consult. The SVT looked just like his underlying left bundle branch block and would start and stop – usually with a PAC. He was administered 2.5mg metoprolol intravenously and loaded with Amiodarone. His SVT became a non-issue thereafter.
He was 70 with critical aortic stenosis and ejection fraction of 10%, coronary artery disease and history of 5-vessel bypass in 2001, a history of Stage D colon cancer with lung mets resected 18 months ago, obesity, diabetes mellitus, chronic renal insufficiency and was recently extubated after a failed aortic valvuloplasty. He later developed a wide complex tachycardia at 150 beats per minute for which I was asked to consult. The SVT looked just like his underlying left bundle branch block and would start and stop – usually with a PAC. He was administered 2.5mg metoprolol intravenously and loaded with Amiodarone. His SVT became a non-issue thereafter. But I didn’t check his HbA1c.
I didn’t check his LDL lipid level.
I didn’t do a diabetic fundoscopic exam.
I didn’t refer him to a neurologist for his mild peripheral neuropathy.
I didn’t get him an evaluation of his footwear.
I didn’t give him an implantable defibrillator or biventricular pacemaker.
I didn’t do universal weight screening.
Instead, I just practiced medicine.
I wonder what my PQRI measure score sheet will look like? I probably won't get my 1.5% bonus from Medicare, I guess. * Sigh *
Too bad there’s no box on that scoresheet for how much money careful judgment could save our healthcare system.
-Wes
The Ultimate Paradox
I found this note in my e-mail this morning:
The good news: the condition was recognized early.
The bad news: the condition was recognized early.
-Wes
"My sister’s 3 sons (my nephews, ages 13, 11 and 8) were all diagnose(d) today with the same heart condition I have: Long QT Syndrome. Please pray for their peace & strength and for the wisdom of all doctors who see and test the boys.Positive congenital screening tests result in the ultimate paradox for the patients and families affected by the results:
They are facing years of tests, possible tachycardia and cardiac arrests, pacemakers, medications."
The good news: the condition was recognized early.
The bad news: the condition was recognized early.
-Wes
Thursday, July 24, 2008
Atrial Fibrillation Podcast
I did an hour-long radio show on atrial fibrillation (afib) yesterday afternoon with my colleague Dr. Jose Nazari, MD. The podcast is now up and you can download it here. If you're brave enough to sit through the hour-long show, you can hear all kinds of tidbits: like what I do for my day job, what afib is, where the name "warfarin" came from, treatment options, and coffee's effects on afib, etc.
If you you don't have time to listen to this, or if you have other questions, I'll also be doing a live on-line chat for an hour on August 6th, 2008 at 7PM central standard time. You can request an e-mail reminder here to log on here. We'll see how fast my fingers can type...
-Wes
If you you don't have time to listen to this, or if you have other questions, I'll also be doing a live on-line chat for an hour on August 6th, 2008 at 7PM central standard time. You can request an e-mail reminder here to log on here. We'll see how fast my fingers can type...
-Wes
Change of Shift is Up With Great Content
Kim over at Emergiblog once again hosts Change of Shift - the best of the nursing blog-o-sphere this week. In it, I found this hilarious depiction of a German doctor's clever way to dance his way in to teaching arrhythmias. Be sure to check out atrial fibrillation and the successful defibrillation:
Enjoy!
-Wes
Enjoy!
-Wes
Wednesday, July 23, 2008
Digitek and Heparin Suits - Forthcoming?
In-pharma Technologist.com has a good review of the Wyeth v. Levine case before the Supreme Court that, like the Riegel v Medtronic case for the medical device industry, will rule if FDA approval of pharmaceutical manufacturing and labeling processes would preempt state liability claims from the recent digitek (digoxin) and heparin manufacturing problems.
-Wes
-Wes
Olympics Fever
Boy, the marketing departments are into the Olympic Spirit! I mean, Triple Gold?
It was quite a feat:
All for a spot on PRNewswire that's picked up by Marketwatch.
It makes you wonder where our money goes, doesn't it?
-Wes
It was quite a feat:
To receive Triple Gold recognition, Aurora St. Luke's Medical Center had to meet 85 percent of performance measures, in all three categories, for two or more years.Just think of the manpower, the cost, the countless hours devoted to non-patient care to assemble this crown.
All for a spot on PRNewswire that's picked up by Marketwatch.
It makes you wonder where our money goes, doesn't it?
-Wes
The Complexities of Controlling Costs in Healthcare
Jim Stergious of the Pioneer Institute wants Massachusetts hospitals to do their part to help pay for the estimated $153 million budget shortfall for the Massachusetts universal healthcare plan:
Unfortunately, we can't have our cake unless we're willing to eat it, too.
The question becomes: what are we eating? Transparency of healthcare costs is one avenue to understand which side of this debate should give. Until we know what healthcare really costs to deliver and avoid the bizarre game of cat and mouse between insurers and hospitals with their Byzantine price markup scheme that confuses the all-important Big Picture of costs, patients (and taxpayers) will continue to get the short shrift.
-Wes
We are already well into the new fiscal year, and negotiations with the federal government continue over whether it will renew the waiver that facilitated the Commonwealth's healthcare experiment in the first place. It might be useful to remember that no matter how conceptually interesting, even idea-based reforms face the logic of mathematics. They have to be affordable.Paul Levy, CEO of Beth Israel Deaconess Medical Center and member of the Cambridge Health Alliance, isn't too pleased with the idea:
The Education Reform Act of 1993 required the grit of legislators and the governor to make good on the promised massive funding increase needed to make it viable. And now we must remain faithful to the idea of the Healthcare Reform Act, or the federal government will kill it.
The government wants reform, and it doesn't want it to affect federal coffers. Reform is happening; we have successfully signed up hundreds of thousands who were previously uninsured. One has to assume that the reduction in the number of people showing up to emergency rooms without insurance is translating into less of a burden on hospitals, especially those that previously provided care to a disproportionate share of the uninsured - specifically Boston Medical Center and Cambridge Health Alliance.
To remain cost-neutral to the federal government, we have to address this year's shortfall of $153 million and a minimum shortfall of $184 million next year. In the long term, there are several things we can do to contain healthcare costs, including perhaps a hard look at certain benefits mandated in the law and increasing the transparency of cost and quality data useful to consumers.
But there is really only one way to address the costs of the legislation in the immediate term: reduce the level of extra payments to Boston Medical Center and Cambridge Health Alliance, which were granted special annual payments that began at $200 million and ratchet down by $20 million a year. These special institutional payments were meant to ease the hospitals into the new regime. They were also very much a political deal.
If we want to keep this new system in place, there are only three sources of revenue for these costs: The taxpayers, the insurance companies and through them their subscribers, and the hospitals. None of these have tremendous political support, and there will be interesting political debates and compromises on Beacon Hill as this is figured out. I am afraid, though, that Jim has mistakenly chosen to avoid the first two and then focused his solution on a subset of the last one.He later relents to the obvious in the comments section:
Tim, of course, is correct that ultimately all flows back from the taxpayers. The policy choice before the Legislature is whether you want to collect that as a direct tax or an indirect tax. Most likely, we will see it hidden as an indirect tax, for the obvious reasons!Yes, the obvious reason: it's politically impossible to have transparency of healthcare costs.
Unfortunately, we can't have our cake unless we're willing to eat it, too.
The question becomes: what are we eating? Transparency of healthcare costs is one avenue to understand which side of this debate should give. Until we know what healthcare really costs to deliver and avoid the bizarre game of cat and mouse between insurers and hospitals with their Byzantine price markup scheme that confuses the all-important Big Picture of costs, patients (and taxpayers) will continue to get the short shrift.
-Wes
Tuesday, July 22, 2008
Grand Rounds is Up
GruntDoc, the infamous Marine-turned-ER doc, serves as host for the sixth time (sheesh!) of the best of the medical blog-o-sphere in the (drum roll, please) 200th edition of Grand Rounds. There's something for everyone.
Enjoy.
-Wes
Enjoy.
-Wes
On Statins and Cancer
The recently-released Simvastatin and Ezetimibe in Aortic Stenosis (SEAS) trial, a placebo-controlled study that examined the reduction in mortality and morbidity of patients with aortic stenosis taking ezetimibe (ZETIA) and simvastatin 40 mg, came with an unexpected finding: a higher-than-expected rate of cancer in the treatment arm compared to the placebo arm of the trial. Almost immediately, the business community stated:
In the PROSPER trial, new cancer diagnoses were more frequent on pravastatin than on placebo (1.25, 1.04-1.51, p=0.020). Also, the CARE trial demonstrated a larger incidence of breast cancer diagnosis in the treatment group as compared to the placebo group. Other statins (specifically simvastatin and lovastatin), interestingly, have not been found to induce cancers. Some researchers have suggested this is because of the lipophylic (fat soluble) nature of those statins, compared the the hydrophyllic (water soluble) nature of pravastatin. Given the results of other studies, simvastatin might not be the culprit.
So what about ezetimibe? Or could the combination of the two drugs simvastatin and ezetimibe have an unexpected synergistic cancer-promoting effect? We really don't know. Certainly, the incidence and diversity of cancers indentified makes causation unlikely, but there are other studies that suggest that perhaps this relationship should be investigated further. For instance, in rodents, lowering of serum cholesterol by the unabsorbed bile acid–binding resin cholestyramine has been shown to promote mammary gland carcinogenesis.
So while I'm willing to accept the premise that the relationship of carcinogenesis is unknown with the simvastatin/ezetimibe combination, given the prior art of research available, I'm not sure I'm willing to write off the potential for a relationship as "implausible."
-Wes
The cancer finding was subjected to a series of analyses by a prominent research team at Oxford University in the United Kingdom. The researchers declared the finding "implausible" and probably the result of chance.While their analysis might be true, when we look at the potential for this "implausibility," it is useful to recall that another statin generated the same "implausible" cancer findings: pravastatin.
...
The data were given to a separate research group from Oxford University's Clinical Trial Service program. Sir Richard Peto, co-director of the program, analyzed the findings over the weekend. He reported during the London news conference that several factors, including the fact that patients had several different types of cancers and that there wasn't any increased incidence over time, convinced him that any real link between Vytorin and cancer was highly unlikely.
In the PROSPER trial, new cancer diagnoses were more frequent on pravastatin than on placebo (1.25, 1.04-1.51, p=0.020). Also, the CARE trial demonstrated a larger incidence of breast cancer diagnosis in the treatment group as compared to the placebo group. Other statins (specifically simvastatin and lovastatin), interestingly, have not been found to induce cancers. Some researchers have suggested this is because of the lipophylic (fat soluble) nature of those statins, compared the the hydrophyllic (water soluble) nature of pravastatin. Given the results of other studies, simvastatin might not be the culprit.
So what about ezetimibe? Or could the combination of the two drugs simvastatin and ezetimibe have an unexpected synergistic cancer-promoting effect? We really don't know. Certainly, the incidence and diversity of cancers indentified makes causation unlikely, but there are other studies that suggest that perhaps this relationship should be investigated further. For instance, in rodents, lowering of serum cholesterol by the unabsorbed bile acid–binding resin cholestyramine has been shown to promote mammary gland carcinogenesis.
So while I'm willing to accept the premise that the relationship of carcinogenesis is unknown with the simvastatin/ezetimibe combination, given the prior art of research available, I'm not sure I'm willing to write off the potential for a relationship as "implausible."
-Wes
Monday, July 21, 2008
Surgical Schmear
The surgical scrub sink is being replaced with schmear.
The days of slathering povidone iodine or chlorhexidine solution over your hands and scrubbing your hands for 3-5 minutes with a soapy watery mess dripping from your elbows as you enter the procedure room or operating room no longer flies. Instead, you get to don “emollients” that stick like gooey glue to your hands and provide continuous “kill” to the bacteria throughout the surgical case. It seems there’s some industry-sponsored research that proves its improved bacterial kill rate. Just wipe in on your dry hands (yes, doctor, they must the dry), let the alcohol evaporate, and slide on those gloves! Total prep time – about 15 seconds. Fast, efficient, effective and relatively cheap.
What could be better?
But it was shocking to find this little orange dispenser next to the scrub sink (arrow) and my usual water-based soap dispenser removed:

Now, I look at our poor scrub sink. Lonely, cold, dull stainless steel. Who will love it when water no longer flows there? Instead, I now look down at my hand after squirting a bit of this slime there and wonder about its uncanny resemblance to… oh, never mind…

All in all, it’s been a paradigm shift in the way I prep for cases. Yes, it's faster. But there's never enough of this stuff to cover your hands and arms with one little squirt. And I ask myself, is it better for the patient? I'm not sure - it's just too early to tell. But one thing's for sure: the residue that remains bound to my hands at the end of each case is most disconcerting - bound for eternity to my dermis so that super-resistant organisms grow on my keyboard.
Why do I know this?
Because I no longer have any regular soap available to wash this stuff off.
-Wes
Ref: Guidelines for Hand Hygiene in Health-care Settings (pdf): Recommendations of the Healthcare Infection Control Practices Advisory Committee and the ICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force, Morbidity and Mortality Weekly Report. October 25, 2002 / Vol. 51 / No. RR-16.
The days of slathering povidone iodine or chlorhexidine solution over your hands and scrubbing your hands for 3-5 minutes with a soapy watery mess dripping from your elbows as you enter the procedure room or operating room no longer flies. Instead, you get to don “emollients” that stick like gooey glue to your hands and provide continuous “kill” to the bacteria throughout the surgical case. It seems there’s some industry-sponsored research that proves its improved bacterial kill rate. Just wipe in on your dry hands (yes, doctor, they must the dry), let the alcohol evaporate, and slide on those gloves! Total prep time – about 15 seconds. Fast, efficient, effective and relatively cheap.
What could be better?
But it was shocking to find this little orange dispenser next to the scrub sink (arrow) and my usual water-based soap dispenser removed:

Now, I look at our poor scrub sink. Lonely, cold, dull stainless steel. Who will love it when water no longer flows there? Instead, I now look down at my hand after squirting a bit of this slime there and wonder about its uncanny resemblance to… oh, never mind…

All in all, it’s been a paradigm shift in the way I prep for cases. Yes, it's faster. But there's never enough of this stuff to cover your hands and arms with one little squirt. And I ask myself, is it better for the patient? I'm not sure - it's just too early to tell. But one thing's for sure: the residue that remains bound to my hands at the end of each case is most disconcerting - bound for eternity to my dermis so that super-resistant organisms grow on my keyboard.
Why do I know this?
Because I no longer have any regular soap available to wash this stuff off.
-Wes
Ref: Guidelines for Hand Hygiene in Health-care Settings (pdf): Recommendations of the Healthcare Infection Control Practices Advisory Committee and the ICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force, Morbidity and Mortality Weekly Report. October 25, 2002 / Vol. 51 / No. RR-16.
Sunday, July 20, 2008
When Radiology Comes to Airport Security

... it can lead to all sorts of interesting findings:
The new full-body imaging machines that will arrive at O'Hare this fall look through clothing to create an explicit silhouette of the traveler—showing shapes, folds of fat and other anatomical characteristics—to identify possible hidden objects.Quick! Where's HIPAA?!? Imagine the breast implants, tummy tucks, pacemakers, defibrillators, mastectomy scars, colostomy bags, naval (and other appendage) jewelry, folds of fat, type of underwear they'll see. Worse yet, what if someone's going "commando" without underwear?!
Even though facial features are blurred to protect privacy, the images reveal breasts, buttocks and other private parts, prompting some civil liberties groups to call the machines an unacceptable intrusion. ...
The full-body imaging pictures are formed by one of two ways—bouncing beams of radio frequency energy off the skin or conducting a low-dose X-ray of an individual.
Man, those poor airport security agents are going to need hazardous duty pay...
... oh, yeah, I forgot to mention...
... welcome to our world.
-Wes
Thursday, July 17, 2008
Meadows Disease
With the passing of a local cardiologist, I learned something today: another name for peripartum cardiomyopathy.
-Wes
Reference: Meadows WR. "Idiopathic Myocardial Failure in the Last Trimester of Pregnancy and the Puerperium." Circulation. 1957;15:903.
-Wes
Reference: Meadows WR. "Idiopathic Myocardial Failure in the Last Trimester of Pregnancy and the Puerperium." Circulation. 1957;15:903.
Six Million Gloves a Year
... it's just one reason oil prices are effecting healthcare costs:
While a single glove can amount to pennies, that cost adds up for a hospital. Medline says it's not uncommon for a 200-bed hospital to use 16,000 gloves a day, or about 6 million a year at a cost of $200,000 a year. A hospital that paid $2.70 two years ago for a box of 100 latex gloves might pay $3.50 to $3.80 today.-Wes
Why Medicine Needs Medical Students
Because they open our eyes to technology's limitations and prompt some corporations to weigh in.
-Wes
-Wes
Wednesday, July 16, 2008
Happy Cost of Government Day!
Yep, there is such a thing:
-Wes
Tax Freedom Day was April 23rd. That's when the average American effectively finished paying taxes to government at all levels. But only the average American. Anyone living in a high-tax state, such as Connecticut, New Jersey, and New York, had to work another couple weeks for government.Can't wait to see what the date will be in four more years after we add more healthcare benefits to the mix...
But taxes are a poor measure of the total cost of government. Because of sizable and persistent deficits, total public spending is a better standard of what we pay for government. Even that isn't enough, however. Regulation adds another substantial charge to the bill.
Americans for Tax Reform adds these together to come up with Cost of Government Day. That's when we really stop paying for government. Last year COGD was July 12. It advanced four days this year to July 16. Explains ATR: "In other words, the cost of government consumes 53.9 percent of national income."
-Wes
It's the End of the World As We Know It
"It's the end of the world as we know it.
It's the end of the world as we know it.
It's the end of the world as we know it and I feel fine."
- REM
The rising cost of healthcare is now taking its toll:
But GM's announcement Tuesday that it would cease medical coverage for its salaried retirees age 65 and above signals that a new era of ever-shrinking benefits has arrived. Beginning in January, even former employees who are already in retirement will lose their benefits, which most of the company's retirees use to supplement gaps in their traditional Medicare coverage. The auto maker will boost monthly pension payouts to help offset the cuts. The company's unionized workers aren't affected by the cut to retiree health benefits.The ripple effect will soon be felt far and wide, as other large companies, saddled with declining bottom lines, will follow suit.
GM isn't the first company to do this, but its heft and influence could help usher in further cutbacks at other companies.
And Congress, in their ever-deflecting manner, will eventually have to come to their senses and scrap the Medicare reimbursement mechanism as it exists today.
But after deflecting the issue yet again, at least they won't have to worry about this for another 18 months.
-Wes
Tuesday, July 15, 2008
CT Scanners and Pacemakers
Well, the phone lines were jumping today. It seems the FDA has issued a "Preliminary Public Health Notification" that CT scanners might cause some medical devices, including pacemakers and defibrillators, to "malfunction:"
Recall that pacemakers must sense existing heartbeats and respond with pacing when no signals are detected. If the pacemaker or defibrillator senses outside signals, it might interpret that "noise" as a biologic signal and respond accordingly. So, if a pacemaker senses outside "noise" and interprets it as a biologic signal, it might briefly inhibit pacing. If a defibrillator senses such "noise" as a biologic signal, it might either inhibit pacing or, if the noise detected is of a sufficiently high frequency for long enough, it might respond with an attempt to correct the rhythm by rapid pacing or a shock (depending on how the defibrillator was programmed).
From the FDA's announcement, it appears the problem primarily occurs when a high radiation dose is emitted from the scanner directly over the device - and this is usually only a brief phenomenon. Whether is is a new finding, or just better reported, remains to be seen (I suspect the latter).
The biggest impact of this announcement will be for device companies and EP nurses, doctors, and technicians - since the implication from this disastrous "early notification" is that we might have to check every pacemaker or defibrillator after every CT scan performed (you've got to be kidding me!).
The lack of guidance for heart rhythm specialists by the FDA and the Heart Rhythm Society in this regard is stunning and warrants review. It seems the Heart Rhythm Society just parrots the FDA's announcement. Perhaps it was because maybe it's not such a big deal after all:
I guess thanks to the Congressional oversight these days, when it comes to such notifications, the FDA is damned if they do and damned if they don't.
-Wes
Most patients with electronic medical devices undergo CT scans without any adverse consequences. However, FDA has received a small number of reports of adverse events in which CT scans may have interfered with electronic medical devices, including pacemakers, defibrillators, neurostimulators, and implanted or externally worn drug infusion pumps. There have been similar reports in the literature.Specifically, for pacemakers, the effect has been described only as "transient changes in pacemaker output pulse rate."
It is possible that this interference is being reported more frequently now because of the increased utilization of CT, the higher dose-rate capability of newer CT machines, an increase in the number of patients with implanted and externally worn electronic medical devices, and better reporting systems.
We are continuing to investigate this issue while working with device manufacturers and raising awareness in the healthcare community. To date, no patient deaths have been reported from CT scanning of implanted or externally worn electronic medical devices.
Recall that pacemakers must sense existing heartbeats and respond with pacing when no signals are detected. If the pacemaker or defibrillator senses outside signals, it might interpret that "noise" as a biologic signal and respond accordingly. So, if a pacemaker senses outside "noise" and interprets it as a biologic signal, it might briefly inhibit pacing. If a defibrillator senses such "noise" as a biologic signal, it might either inhibit pacing or, if the noise detected is of a sufficiently high frequency for long enough, it might respond with an attempt to correct the rhythm by rapid pacing or a shock (depending on how the defibrillator was programmed).
From the FDA's announcement, it appears the problem primarily occurs when a high radiation dose is emitted from the scanner directly over the device - and this is usually only a brief phenomenon. Whether is is a new finding, or just better reported, remains to be seen (I suspect the latter).
The biggest impact of this announcement will be for device companies and EP nurses, doctors, and technicians - since the implication from this disastrous "early notification" is that we might have to check every pacemaker or defibrillator after every CT scan performed (you've got to be kidding me!).
The lack of guidance for heart rhythm specialists by the FDA and the Heart Rhythm Society in this regard is stunning and warrants review. It seems the Heart Rhythm Society just parrots the FDA's announcement. Perhaps it was because maybe it's not such a big deal after all:
MedSun is the FDA's Medical Product Safety Network of 350 hospitals spread throughout the United States. Information from 132 of these facilities indicated that they have not experienced any CT medical device interference, while 3 have had from 1 to 3 events that may have been CT scan induced. Fifteen MedSun facilities indicated they take some precautionary steps when CT scanning patients who have electronic medical devices.In short, this seems like a "cover your ass" move by the FDA that threatens to potentially scaremonger our patients.
I guess thanks to the Congressional oversight these days, when it comes to such notifications, the FDA is damned if they do and damned if they don't.
-Wes
It's Official: University of Chicago Joins With ENH
Evanston Northwestern Healthcare (ENH) and University of Chicago will join hands to train U of Chicago medical students.
For the Northwestern University medical students we currently train, the feelings are mixed. Perhaps this is fear of the unknown. Perhaps the feelings are justified. I spoke with a third-year medical student who felt that the ripple effect has already taken hold and worries that their training will be viewed differently when they apply for jobs. What is clear, is how vulnerable they feel during the upcoming transition period and the uncertainty of their continued training.
For faculty members here at ENH, too, many questions remain: what will be the new name of ENH? (Expect an announcement soon, now that ENH can move on.) What benefits for faculty members will convey from the former Northwestern affilitation agreement to the new affiliation agreement with U of Chicago? Who will keep their academic appointments and who will lose them?
One thing's for sure: there'll be lots of changes. Let's hope they're for the better.
-Wes
For the Northwestern University medical students we currently train, the feelings are mixed. Perhaps this is fear of the unknown. Perhaps the feelings are justified. I spoke with a third-year medical student who felt that the ripple effect has already taken hold and worries that their training will be viewed differently when they apply for jobs. What is clear, is how vulnerable they feel during the upcoming transition period and the uncertainty of their continued training.
For faculty members here at ENH, too, many questions remain: what will be the new name of ENH? (Expect an announcement soon, now that ENH can move on.) What benefits for faculty members will convey from the former Northwestern affilitation agreement to the new affiliation agreement with U of Chicago? Who will keep their academic appointments and who will lose them?
One thing's for sure: there'll be lots of changes. Let's hope they're for the better.
-Wes
Monday, July 14, 2008
Messin' With People
Should news stories about new unproven innovations in medicine be reported in the mainstream media as though they were already safe and effective?
It's an age-old problem, but one that warrants revisiting.
Certainly for the companies developing the technology, there is a desire to find patients who might be good candidates for a clinical trial that tests the new device. Companies have limited budgets to negotiate the complicated regulatory environment of the Food and Drug Administration (FDA) in their quest to acquire approval for the sale of their device. So if a little "press release" escapes to the media about the new technology, well, all the better.
For the researchers, there are often powerful financial and academic incentives to being the most experienced individual in medicine with a new technology is launched: patients learn of one's expertise and the researcher gains first access to the data from the clinical trial permitting an opportunity for the researcher to be "first author" on the sentinel paper describing the technology in a major medical journal. Reputations are made in our profession by such notoriety.
Hospitals and research institutes, too, are constantly looking for more funds to grow their "foundations." Donors are urged to contribute to their next endeavors, holding their best and brightest researchers forward at their rubber-chicken fund-raisers.
For news agencies, too, the push to acquire new and interesting content for their readers and viewers improves readership and advertising revenues. Nearly always, the news outlets are interested in the "human interest" aspect of the technology: how does it affect the Average Joe? So they seek out a patient who has benefited from the technology to tell the story. "Doctor, do you have a patient who could describe their experience using this new gizmo?"
And there begins the problem.
Well-meaning doctors gush forth with the name of their favorite patient experience. The patient is called, tells the "Best Story Ever" and is affable and approachable. The media bring their lights, cameras, and sound equipment to the hospital. Patients and doctors feel important, valued. The marketing opportunity, the public relations benefit, the cache' of being the most cutting edge - it's all so sexy. Everybody's happy. Ahhhh, the glory! What's not to like?
Unfortunately, plenty.
There is much to lose by such PR. This practice of early reporting of technologies before they are proven safe or effective introduces unprecedented bias in to any trial: bias for the research subjects, bias of the researcher's perceptions of the technology, and bias for the public at large. The patient who didn't fare so well is never brought forward - this would too unseemly for the institution, the doctor-researcher, and the company's aspiration to sell their device. Unless trials are prospective, randomized, multi-center trials, it is rare to have negative results reported in the literature, since it is much harder to right about what went wrong than what went right. Who wants that scarlet letter on their resume'?
Clinical researchers have an obligation to tell our patients the good, the bad and the ugly about any new innovation. Certainly no one wants to short-change the opportunity for patients to know about new innovations that might help their condition. But a 90-second feel-good sound bite in the media is just not the place to do that.
Ever.
-Wes
It's an age-old problem, but one that warrants revisiting.
Certainly for the companies developing the technology, there is a desire to find patients who might be good candidates for a clinical trial that tests the new device. Companies have limited budgets to negotiate the complicated regulatory environment of the Food and Drug Administration (FDA) in their quest to acquire approval for the sale of their device. So if a little "press release" escapes to the media about the new technology, well, all the better.
For the researchers, there are often powerful financial and academic incentives to being the most experienced individual in medicine with a new technology is launched: patients learn of one's expertise and the researcher gains first access to the data from the clinical trial permitting an opportunity for the researcher to be "first author" on the sentinel paper describing the technology in a major medical journal. Reputations are made in our profession by such notoriety.
Hospitals and research institutes, too, are constantly looking for more funds to grow their "foundations." Donors are urged to contribute to their next endeavors, holding their best and brightest researchers forward at their rubber-chicken fund-raisers.
For news agencies, too, the push to acquire new and interesting content for their readers and viewers improves readership and advertising revenues. Nearly always, the news outlets are interested in the "human interest" aspect of the technology: how does it affect the Average Joe? So they seek out a patient who has benefited from the technology to tell the story. "Doctor, do you have a patient who could describe their experience using this new gizmo?"
And there begins the problem.
Well-meaning doctors gush forth with the name of their favorite patient experience. The patient is called, tells the "Best Story Ever" and is affable and approachable. The media bring their lights, cameras, and sound equipment to the hospital. Patients and doctors feel important, valued. The marketing opportunity, the public relations benefit, the cache' of being the most cutting edge - it's all so sexy. Everybody's happy. Ahhhh, the glory! What's not to like?
Unfortunately, plenty.
There is much to lose by such PR. This practice of early reporting of technologies before they are proven safe or effective introduces unprecedented bias in to any trial: bias for the research subjects, bias of the researcher's perceptions of the technology, and bias for the public at large. The patient who didn't fare so well is never brought forward - this would too unseemly for the institution, the doctor-researcher, and the company's aspiration to sell their device. Unless trials are prospective, randomized, multi-center trials, it is rare to have negative results reported in the literature, since it is much harder to right about what went wrong than what went right. Who wants that scarlet letter on their resume'?
Clinical researchers have an obligation to tell our patients the good, the bad and the ugly about any new innovation. Certainly no one wants to short-change the opportunity for patients to know about new innovations that might help their condition. But a 90-second feel-good sound bite in the media is just not the place to do that.
Ever.
-Wes
Saturday, July 12, 2008
Time Critical Healthcare
Gosh, a while ago I published this tongue-in-cheek piece about feeding the beast of healthcare and this piece about the complexities of the 90-minute door-to-balloon (D2B) time for a heart attack treatment. I had no idea that others would actually take me seriously:
-Wes
House Bill 1790, sponsored by Rep. Robert Wayne Cooper, creates a "Time Critical Diagnosis System" for stroke and ST-elevation myocardial infarction (STEMI), a particularly fatal type of heart attack. Missouri is the first state in the nation to enact legislation governing a STEMI and stroke statewide system of care.Well, since this is D2B time is now a tracked "Pay-for-Performance" measure, I guess it's not surprising that we're circling our wagons and spending countless hours to fufill the government's expectations. But the data upon all of this wild excitement rests is based on "hospital door" to "balloon" time, not "patient's door" to "balloon" time. Doctors still need time to assess the complexities of social situations and confounding medical issues. Should a patient with widely disseminated cancer who also has an acute heart attack recieve similar "life-saving" resources? Further, one wonders how much more administrative and bureaucratic overhead our healthcare system can handle for this one initiative. What about the patients already in the ER waiting to be seen? It goes without saying that the administrative complexities of this system are sure to be stunning. Just look at all of the bureaucratic planning:
The health department has already been preparing the state to implement a system of stroke and STEMI centers. A Time Critical Diagnosis Task Force that was formed by the department in November has been meeting to discuss how to build the new system. The task force included more than 100 members of the emergency medicine community.The first question to be answered by the Task Force should be this: when have 100 people in a committee ever fully agreed on anything?
-Wes
Friday, July 11, 2008
Medical Instruction: Dying on the Vine
It's happening more and more:
Then, after being slapped by residency-review committees about their deficiencies and threatened with a sudden drop in federally-mandated funds for teaching, hospitals jump to action:
-Wes
The program to train cardiologists at Los Angeles County-USC Medical Center has been stripped of its national accreditation by the Accreditation Council for Graduate Medical Education. The decision marks the first time a residency or fellowship program at the facility has lost accreditation. The council faulted the program for "insufficient teaching time by the faculty."It's really not unexpected, though. Clinical faculty at medical schools are increasingly pressured to maintain "productivity" standards based on Medicare's RVU system, while rarely being compensated for the time spent teaching students. As a result, training programs suffer.
Then, after being slapped by residency-review committees about their deficiencies and threatened with a sudden drop in federally-mandated funds for teaching, hospitals jump to action:
County-USC hopes to fix the problems and have the 21-year-old cardiology program recertified before June 30, 2009, when the accreditation is to be withdrawn.Teaching subsidies must flow more consistently to the people doing the teaching and not to support the training program "overhead:"
A main argument for reducing IME payments is supported by data demonstrating that teaching hospitals have substantially higher margins on their Medicare business than other hospitals. In 1999, inpatient Medicare margins for all hospitals were, on average, 11.9 percent. For major teaching hospitals this figure was 22.3 percent versus 11.6 percent for other teaching hospitals, and 6.5 percent for non-teaching hospitals.Only when such transparency is evident to the instructors will there be a long-term incentive to maintain most clinical training programs.
Finally, some point out that the logic of providing support for the social mission of teaching hospitals under Medicare IME is not rational, and that it is a "disguised" payment that should be more transparent. This argument suggests that these types of payment mechanisms provide little accountability for the funds provided for the social missions of teaching hospitals.
-Wes
Atrial Fibrillation: Let's Chat
As part of our Web 2.0 initiative to discuss health issues with patients, I have agreed to perform an online "live" chat about atrial fibrillation and its diagnosis and treatment options on Wednesday, 6 August 2008 at 7PM, central standard time. Oh, there will be some pre-screening of questions so the usual flame-throwing inherent to the blog-o-sphere can be avoided, but hopefully, it will be informative.
You can request an e-mail reminder so we can torment you, if you'd like. Also, if you want to front-load some questions you'd like addressed on this post, feel free to post them here so I can come prepared.
Lookin' forward to the opportunity...
-Wes
You can request an e-mail reminder so we can torment you, if you'd like. Also, if you want to front-load some questions you'd like addressed on this post, feel free to post them here so I can come prepared.
Lookin' forward to the opportunity...
-Wes
Fragmentation
If you haven’t seen the remarkable management of a medical “never” error that was displayed by Paul Levy, President and CEO of Beth Israel Deaconess Hospital over at Running A Hospital, I’d encourage you to read it. This post should be a “must read” for any hospital risk management personnel or hospital administrator.
In short, this is what happened:
So off went the “physician safety division” to interview all involved while the details regarding the incident were fresh in everyone’s mind. The doctor (appropriately) notified the patient’s family and made a full apology. And the board member chimed in:
I read through the more than 45 responses to Mr. Levy’s remarkable post, and there, at the very bottom, was the one response that stopped the entire thread in it’s tracks, as one brave Noah Zark stepped forward and said:
... we realize what we’ve lost.
-Wes
In short, this is what happened:
It was a hectic day, as many are. Just beforehand, the physician was distracted by thoughts of how best to approach the case, and the team was busily addressing last-minute details. In the midst of all this, two things happened: First, no one noticed that the wrong side was being prepared for the procedure. Second, the procedure began without performing a "time out," that last-minute check when the whole team confirms "right patient, right procedure, right side." The procedure went ahead. The error was not detected until after the procedure was completed.Mr. Levy described the doctor’s, hospital’s and hospital board’s response to the error, which, considering the proverbial cat-was-out-of-the-bag, was commendable. Readers were awestruck by the “openness” and “humanness” of the moment. I confess, I too, was impressed at the handling of a disaster that no one should have to endure. Of course the natural question that arises in such a circumstance is “How could that happen?”
So off went the “physician safety division” to interview all involved while the details regarding the incident were fresh in everyone’s mind. The doctor (appropriately) notified the patient’s family and made a full apology. And the board member chimed in:
"Protocols are meant to make procedures insensitive to distraction and busy days. These are inadequate and embarrassing excuses. The 'culture of safety' has not permeated the front lines. Culture of safety training, and application of advances in safety science, I believe, are critical to preventing the type of complex harm that occurs in hospitals. Not just for new staff. For everyone who wears a BIDMC badge, or is affiliated as a physician to the hospital. I know that this is a new science, and a new way of doing business, but this event might just give that leverage needed for change."There it was. Corporate speak: “culture of safety,” “culture of safety training,” that “hasn’t permeated the front lines”, the era of “new science, and a way of doing business.”
I read through the more than 45 responses to Mr. Levy’s remarkable post, and there, at the very bottom, was the one response that stopped the entire thread in it’s tracks, as one brave Noah Zark stepped forward and said:
”I have an idea. Perhaps the surgeon (as opposed to a PA, NP, intern, or Family Doc) should perform and record the complete pre-op history and physical exam requisite for surgery. This ancient protocol ensures that the surgeon knows the patient for the sake of both...; but it is not followed any more.We all know Mr. Zark is right. We also know that it is unlikely, in today’s day and age of the “business” of medicine, that real change in how care is delivered by physician’s stretched to do more in less time than ever before, will occur. We have become fragmented as a profession – too specialized – too procedurally based - too frenetic to stop and really speak and examine patients like we all learned in medical school. Those values lose their cache in the business world of medicine and is exactly the reason that wrong site surgery exists today. That’s why this error was so sad...
Don't waste your time with high tech digital video that can be played from your state of the art computers...just be sure the surgeon examines the patient before he/she is in the OR...the old fashioned way.”
... we realize what we’ve lost.
-Wes
Thursday, July 10, 2008
Change of Shift - Year Three
Be sure to check out the best of nursing's blogs with Kim over at Emergiblog as the nursing blog carnival "Change of Shift" begins its third year:
-Wes
In celebration, I asked nurse bloggers to send in their first posts and tell us a bit about why they started blogging.Enjoy!
-Wes
Back up and Runnin'
Thanks to our Information Technology department for making this blog and that of my administrative colleague, Tony Chen, available to all at our institution. The firewall issues appear to be resolved.
-Wes
-Wes
Never Mind the Trolling
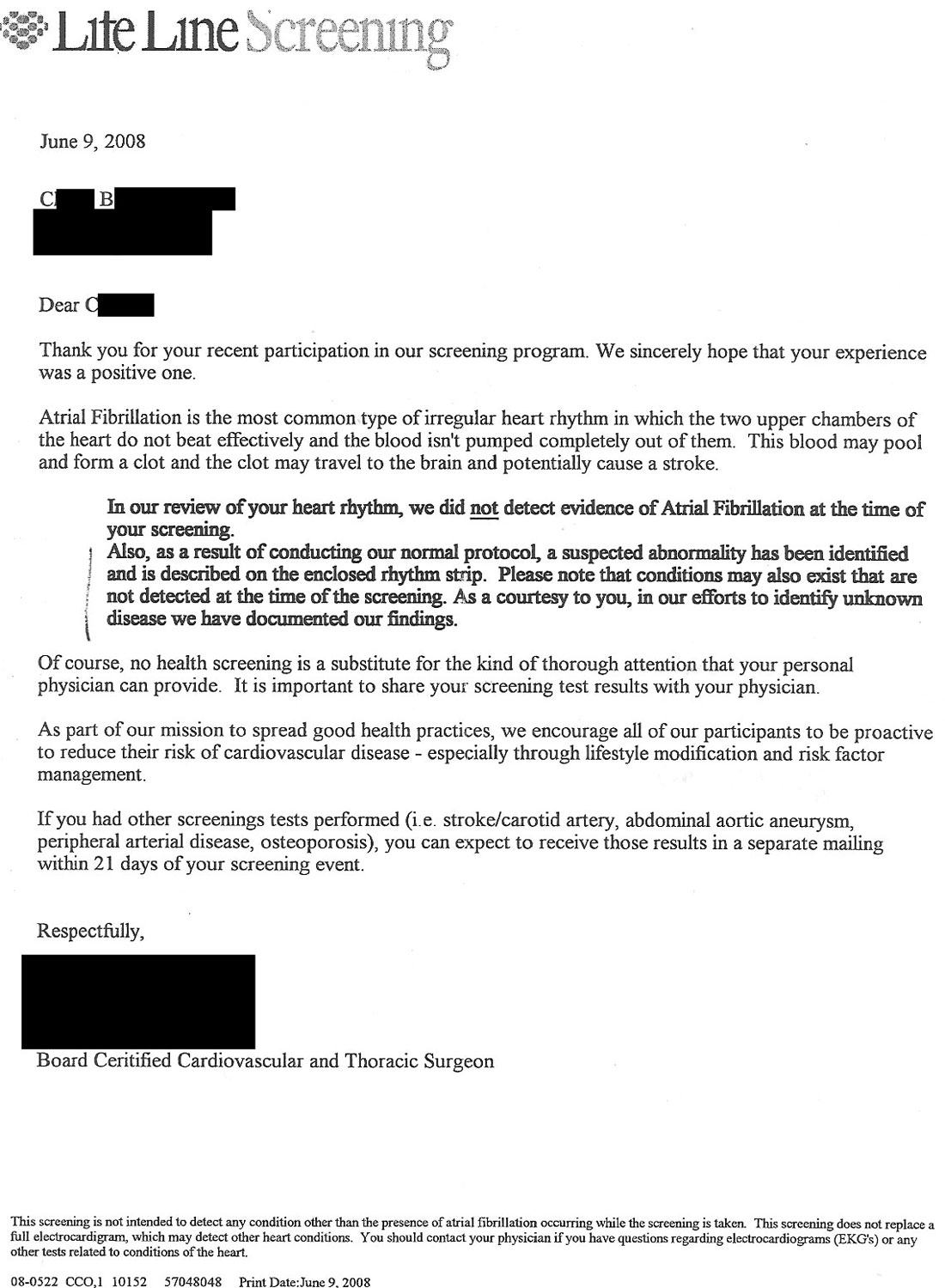
It was just another concerned patient: another victim of a screening test… a patient caught by our trolling net of screening tests for the worried well.
This time is was a “screening” for atrial fibrillation: charged to the patient and their employer under the guise of a corporate “wellness” initiative:
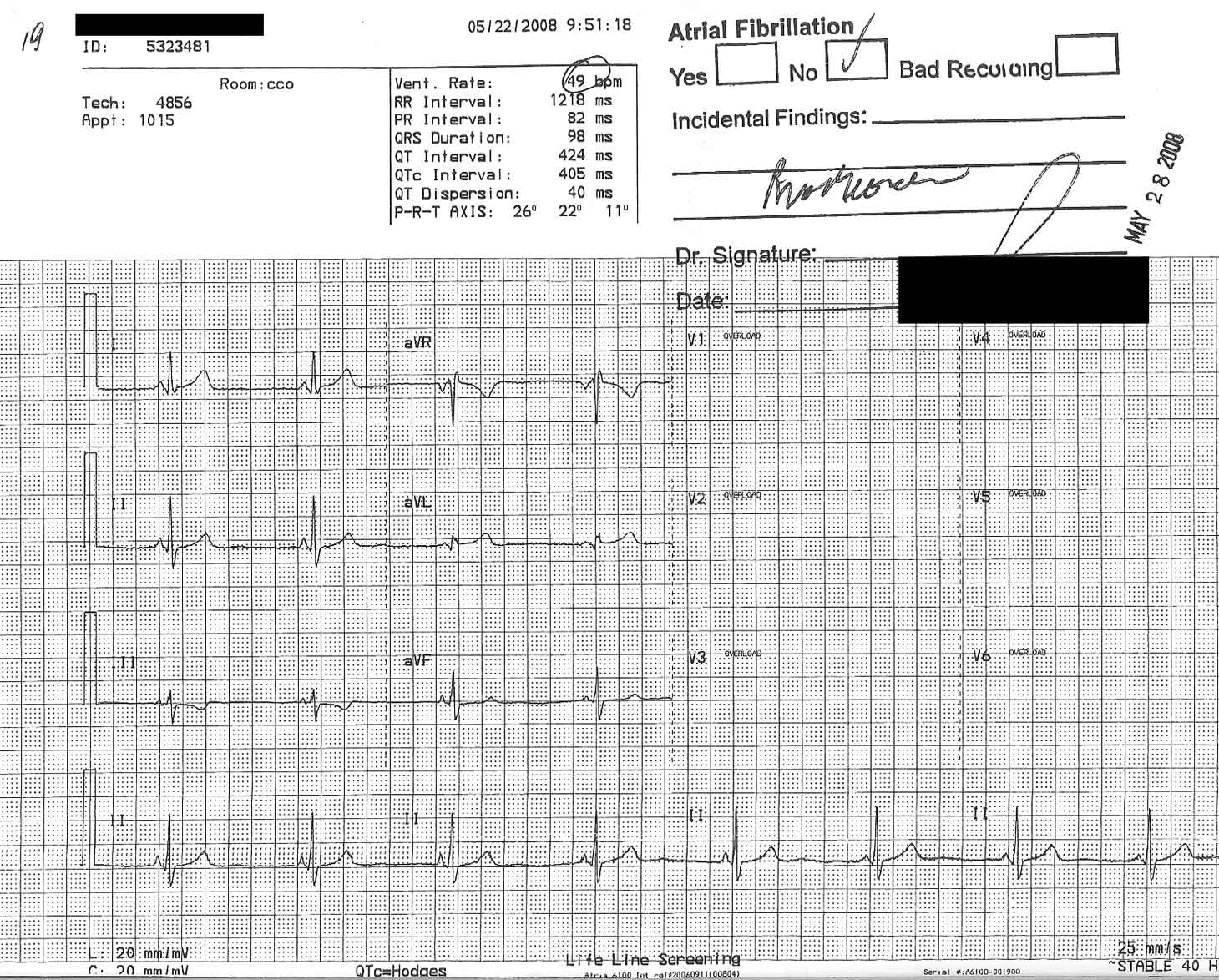
Never mind that the “EKG” wasn’t really an EKG, but rather a “screening” that contained only six of the usual 12 EKG leads, so if an “abnormality” was found, another real EKG would have to be performed.
Never mind that no one would explain the results to her, but rather sent this letter describing a “suspected abnormality” whose findings are “described on the enclosed rhythm strip:”
Never mind that the patient could not read the findings “described on the rhythm strip.”
Never mind that the patient’s short PR interval was not identified.
Never mind the patient already had an EKG in the past and had already had an electrophysiology study (which was normal).
Never mind that the screening company, in their effort to “spread good health practices” fails to mention how to perform “lifestyle modification” or “risk factor management” in their cover letter.
Never mind that all of the other tests performed by the screening company for carotid/stroke, abdominal aortic aneurism, peripheral vascular disease aren’t real tests either, but different “screening tests” that will require more tests if an abnormality is found.
Never mind a cardiac electrophysiologist charges the patient several hundred dollars for “clarification” of the scribbled interpretation of the rhythm strip: “Bradycardia.”
Worse still: never mind that taking a pulse would have served as a much more cost-effective “screening” test for atrial fibrillation in most patients.
Regarding ways to save money to our healthcare system and patients…
… oh, never mind.
-Wes
This time is was a “screening” for atrial fibrillation: charged to the patient and their employer under the guise of a corporate “wellness” initiative:
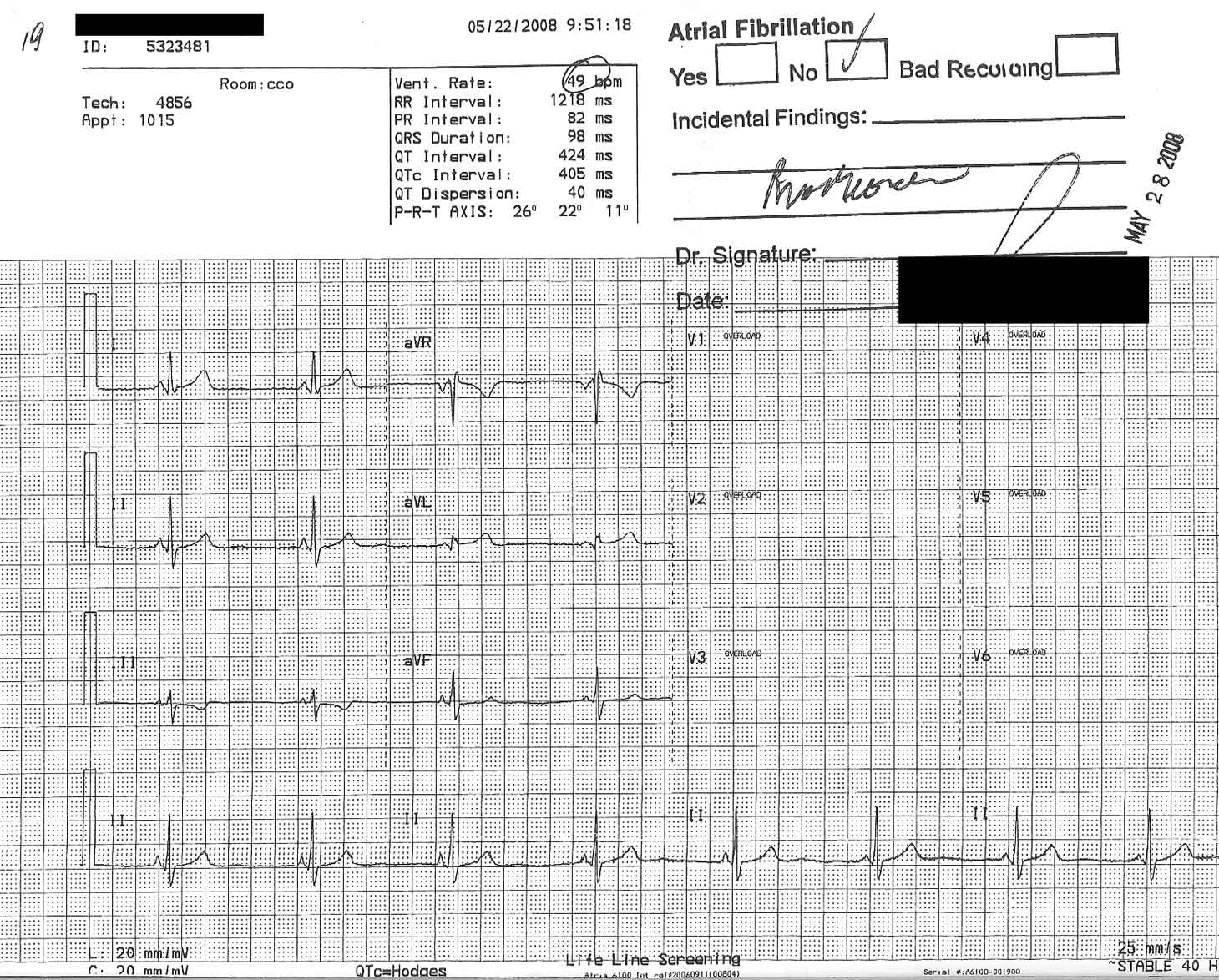
(Click image to enlarge)
Never mind that the “EKG” wasn’t really an EKG, but rather a “screening” that contained only six of the usual 12 EKG leads, so if an “abnormality” was found, another real EKG would have to be performed.
Never mind that no one would explain the results to her, but rather sent this letter describing a “suspected abnormality” whose findings are “described on the enclosed rhythm strip:”
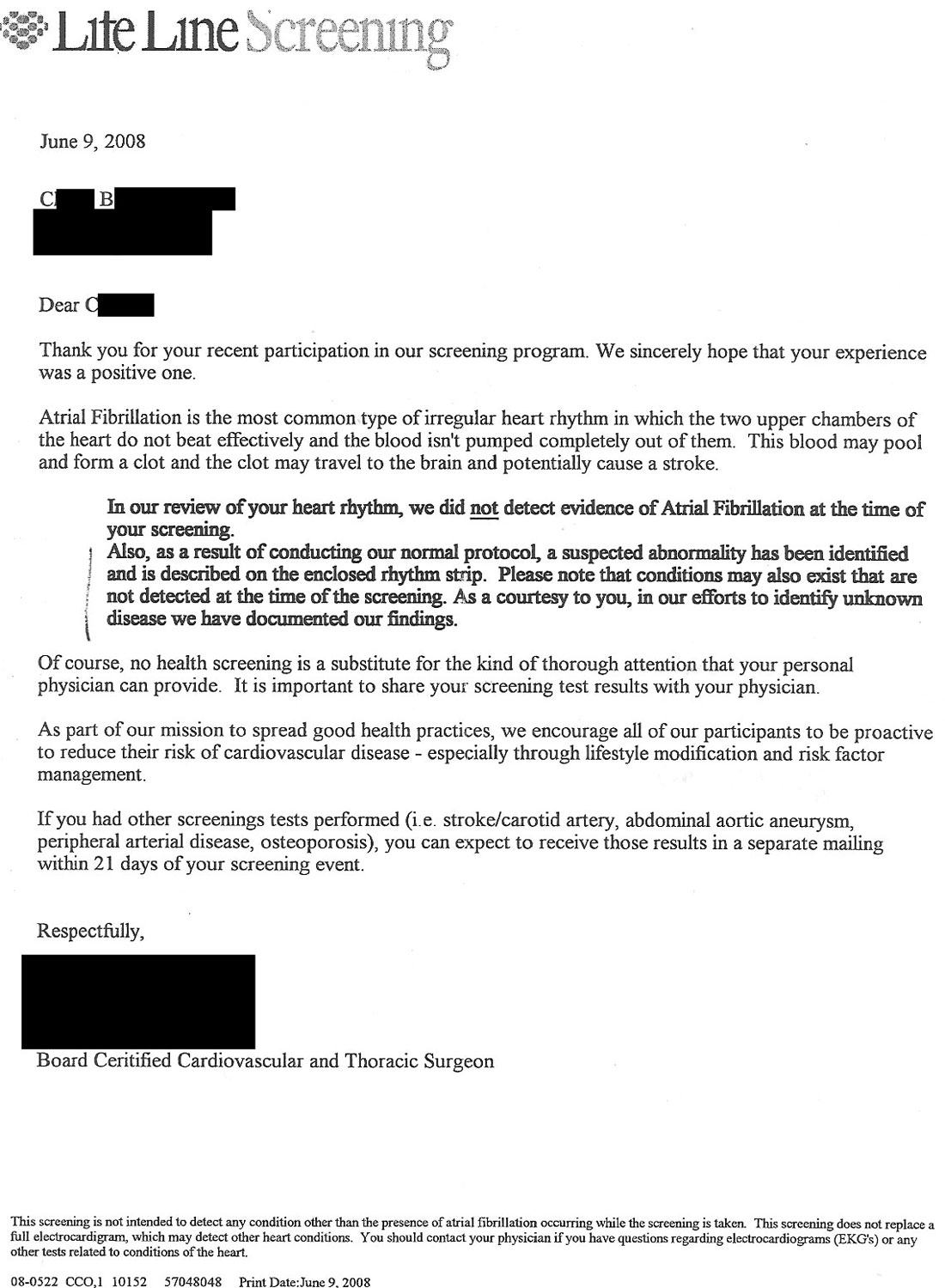
(Click image to enlarge)
Never mind that the patient could not read the findings “described on the rhythm strip.”
Never mind that the patient’s short PR interval was not identified.
Never mind the patient already had an EKG in the past and had already had an electrophysiology study (which was normal).
Never mind that the screening company, in their effort to “spread good health practices” fails to mention how to perform “lifestyle modification” or “risk factor management” in their cover letter.
Never mind that all of the other tests performed by the screening company for carotid/stroke, abdominal aortic aneurism, peripheral vascular disease aren’t real tests either, but different “screening tests” that will require more tests if an abnormality is found.
Never mind a cardiac electrophysiologist charges the patient several hundred dollars for “clarification” of the scribbled interpretation of the rhythm strip: “Bradycardia.”
Worse still: never mind that taking a pulse would have served as a much more cost-effective “screening” test for atrial fibrillation in most patients.
Regarding ways to save money to our healthcare system and patients…
… oh, never mind.
-Wes
Wednesday, July 09, 2008
Tuesday, July 08, 2008
Grand Rounds - The Seinfeld Way
Some of the best moments in Seinfeld (and med-blogging) history are shown ... thanks to TBTAM over at The Blog That Ate Manhattan.
-Wes
-Wes
Why Doctor's Don't Use Electronic Communication
Benjamin Brewer, MD over at the Wall Street Journal gives his take:
-Wes
When it comes to e-visits my patients don't seem to want another password to remember. And they really don't want to pay the $30 I charge for an online consultation and that their insurance doesn't usually cover.For the small, independent practice, Dr. Brewer articulates the barriers to entry for many doctors. Larger health systems, like ours, have heavily-integrated secure communication systems that can transmit test results and facilitate communication without the need for "transaction fees." Until such systems become available (and affordable) to rural docs like Dr. Brewer, widespread adoption of electronic medical record systems will be limited.
Maybe patients don't use our email system because we provide good access by phone and in the office.
In retrospect, I should have surveyed my patients before I spent money on a secure email platform and state-of-the-art software for electronic consults. I guess I was a little too far ahead of the curve.
In some parts of the country doctors are using e-visits and electronic communication to good effect. Some are even getting paid for it. We aren't. Our local insurers, Medicare and Medicaid haven't embraced the idea.
Right now it costs my practice $1,800 a year to maintain our cool Web site. The company that provides it wants a $6 transaction fee for each e-visit, and 50 cents for every appointment and prescription refill I process with their software. We haven't come anywhere near covering our costs.
I checked with another popular company and they wanted a $3.50 cut from each visit. Giving 14% or more of e-visit fees to a transaction processor still seems too much.
The cost is too high for small practices for this to really catch on. The right combination of ease of use, price, security and connectivity to physicians' electronic records systems hasn't been found yet.
-Wes
Monday, July 07, 2008
Pharmaceutical Overreaching?
I stand in awe.
Despite admitting "not 'a whole lot' of data on pediatric use of cholesterol-lowering drugs, recent research showed that the drugs were generally safe for children" and that "average total cholesterol levels as well as LDL and HDL cholesterol have remained stable, while triglyceride levels have dropped, based on data collected from 1988 to 2000" it seems we have an "epidemic" of hypercholesterolemia that now requires drug therapy:
Oops.
Given the unknown implications of statins in pregnancy, one wonders if we should know more before promulgating such far-reaching recommendations.
-Wes
For a more detailed review, please see Sandy Szwarc's recent excellent review following similar recommendations that emanated from the American Heart Association.
Addendum 8 Jul 2008: Statins for kids: the New York Times reconsiders.
Despite admitting "not 'a whole lot' of data on pediatric use of cholesterol-lowering drugs, recent research showed that the drugs were generally safe for children" and that "average total cholesterol levels as well as LDL and HDL cholesterol have remained stable, while triglyceride levels have dropped, based on data collected from 1988 to 2000" it seems we have an "epidemic" of hypercholesterolemia that now requires drug therapy:
The nation’s pediatricians are recommending wider cholesterol screening for children and more aggressive use of cholesterol-lowering drugs starting as early as the age of 8 in hopes of preventing adult heart problems.I can see it now: a young, overweight teenager with a family history of heart disease is placed on a statin drug. She later becomes pregnant.
The new guidelines were to be issued by the American Academy of Pediatrics on Monday.
Oops.
Given the unknown implications of statins in pregnancy, one wonders if we should know more before promulgating such far-reaching recommendations.
-Wes
For a more detailed review, please see Sandy Szwarc's recent excellent review following similar recommendations that emanated from the American Heart Association.
Addendum 8 Jul 2008: Statins for kids: the New York Times reconsiders.
Saturday, July 05, 2008
The Patients Who Cry Wolf
If you want to find out how a hospital of emergency room works, do you send in "secret shoppers?"
-Wes
"As a matter of ethics, you always have to justify why you would need to deceive someone," said Nancy Berlinger, deputy director and a research associate at The Hastings Center, a bioethics research institute in Garrison, N.Y.In a time where ER's are overcrowded, resources are in short supply, doctors and nurses are pushed to their limits, and patients' care is compromised by this fraudulent activity, this monitoring practice should be outlawed.
Questions have also been raised about how far these undercover patients should go, because they could be exposed to procedures and medications that carry real risks.
Earlier this year, an Essex County, N.J., hospital had some of its own employees pose as secret shoppers to see whether nurses were reading back physician medication orders over the phone to ensure accuracy. Protocol also called for the nurses to record the encounter in the patient's chart
A spokesman for the hospital said employees from doctors to technicians were tapped to secretly observe the nurses, then record whether they complied with the rule.
"We discovered there was very high compliance, although it wasn't 100 percent. In those instances where the person was not complying, we just contacted them and informed them we really needed them to do this," spokesman Richard Wells said, adding that no punitive action was taken.
-Wes
Thursday, July 03, 2008
Bummer
Some of our good friends lost their house today.
Sad. Fortunately, they're okay.
Here's pics from the area before the fire. The last one was from their balcony.
-Wes
Addendum: The AP video containing the remnants of their home: just the outline of the foundation and fireplace stonework remained.
Sad. Fortunately, they're okay.
Here's pics from the area before the fire. The last one was from their balcony.
-Wes
Addendum: The AP video containing the remnants of their home: just the outline of the foundation and fireplace stonework remained.
Where Some Hospital Systems Get Their Money
From their friendly neighborhood Congressman and my tax dollar.
It seems hospital construction projects were in vogue last month in Montana: Billings area hospitals got $250,000, Roundup Memorial Hospital got $350,000, Missoula Area Hospitals got $650,000, and Benefis Health System in Great Falls got $700,000 and Sidney Health Center got $100,000.
$2,050,000 to hospitals all from one little bill.
Nothin' like a little pork rider, huh?
-Wes
It seems hospital construction projects were in vogue last month in Montana: Billings area hospitals got $250,000, Roundup Memorial Hospital got $350,000, Missoula Area Hospitals got $650,000, and Benefis Health System in Great Falls got $700,000 and Sidney Health Center got $100,000.
$2,050,000 to hospitals all from one little bill.
Nothin' like a little pork rider, huh?
-Wes
Wednesday, July 02, 2008
Should Teens be Fined for Smoking?
Eric Zorn, syndicated columnist at the Chicago Tribune, likes the PUP laws (laws that ban the "purchase, use and possession" of tobacco by minors) that fine teens for smoking. And he has supporters:
Why do the police and I have to be drawn "into the situation?" Isn't there enough of a power struggle regarding separation going on already in adolescence?
Not only do police have bigger fish to fry, the very people who like such a laws inforced on teens all-too-often will be the same people who pay their own teens' tobacco possesion fines for them.
-Wes
That makes sense, said John Banzhaf, executive director of Washington-based Action on Smoking and Health. PUP laws "serve to draw parents into the situation" and give children an additional reason to resist peer pressure.While I admire his bravery, I beg to differ.
"Treating cigarettes like we do alcohol would go a long way" toward discouraging teen smoking, Banzhaf said. And if you stop a teen from smoking, he said, the odds are overwhelming that he'll never be a smoker.
Why do the police and I have to be drawn "into the situation?" Isn't there enough of a power struggle regarding separation going on already in adolescence?
Not only do police have bigger fish to fry, the very people who like such a laws inforced on teens all-too-often will be the same people who pay their own teens' tobacco possesion fines for them.
-Wes
Grand Rounds for Independence Day
Dr. Rich over at the Covert Rationing Blog carries the flag:
-Wes
This week, bloggers from across the Internet have submitted articles that will help us celebrate the 232nd birthday of the United States of America. Their patriotic postings, organized according to their relationship to the Founding, follow:And it's worth the time just to read his astute interspersed commentary:
Taking into account the bizarre incentives, Byzantine inefficiencies, and systematized grievances that are provided in such luxurious abundance by Medicare, Happy (and DrRich) can only marvel in dazed wonderment that anyone thinks that turning the whole healthcare system over to these people is a good idea. Imagine our honored forebears clamoring to turn over the entire colonial economic system to the perpetrators of the Stamp Act!It makes you want to go out and get yourself a muzzle-loader...
-Wes
Tuesday, July 01, 2008
Grabbin' Us By the Short-hairs
Hey folks! Let’s try a little quiz! I’m going to give you a list of drugs and let’s see if you can guess the diagnosis, okay?
Here are three lists:
1.)Lasix (furosemide), Coreg (Carvedilol), Vasotec (enalapril)
2) metformin, glyburide
3) zidovudine, AZT, azidothymidine, ZDV
Now take your time. Think hard about the answers…. Okay, did you guess:
1) Congestive heart failure
2) Type II diabetes
3) AIDS?
If so, you’re a winner! Way to go!
Now, imagine if every person has every drug they ever took on a single database. Imagine that every doctor in the United States could access that database to assure their patients are on the correct medication. A place where drug coverage information and a list of retail and mail-order pharmacies will be housed under one electronic roof. A place where old drugs, like prior use of psychotropics that might interact with other drugs, could be reviewed. That would be Utopia, right? I mean, fewer errors, more legible scripts generated from that database, an easy-to-update location to stay current on the latest drug information and all.
Now what would such a database be worth? Gosh, I have no idea. Certainly, it wouldn’t be worth much, right? I mean, there wouldn’t be any business potential to such a huge data warehouse, would there? After all, you don’t think an insurer might like to look at that database and you know, guess what illnesses a person has, would they?
Nah, that wouldn’t be worth much. It’d be chump change. It’s be worth so little that even IF the largest electronic prescription warehouses in the world came together to join hands it would be worth so little that the Federal Trade Commission would have to look into them for antitrust practices. Really they wouldn’t. After all it ain’t worth a dime, I mean, they say so:
And why not? Their company won’t be worth much at all (really it won't), Congress will love it, AND they'll effectively have our healthcare system and privacy by the balls.
"Kum-ba-ya, my Lord. Kum-ba-ya..."
-Wes
Here are three lists:
1.)Lasix (furosemide), Coreg (Carvedilol), Vasotec (enalapril)
2) metformin, glyburide
3) zidovudine, AZT, azidothymidine, ZDV
Now take your time. Think hard about the answers…. Okay, did you guess:
1) Congestive heart failure
2) Type II diabetes
3) AIDS?
If so, you’re a winner! Way to go!
Now, imagine if every person has every drug they ever took on a single database. Imagine that every doctor in the United States could access that database to assure their patients are on the correct medication. A place where drug coverage information and a list of retail and mail-order pharmacies will be housed under one electronic roof. A place where old drugs, like prior use of psychotropics that might interact with other drugs, could be reviewed. That would be Utopia, right? I mean, fewer errors, more legible scripts generated from that database, an easy-to-update location to stay current on the latest drug information and all.
Now what would such a database be worth? Gosh, I have no idea. Certainly, it wouldn’t be worth much, right? I mean, there wouldn’t be any business potential to such a huge data warehouse, would there? After all, you don’t think an insurer might like to look at that database and you know, guess what illnesses a person has, would they?
Nah, that wouldn’t be worth much. It’d be chump change. It’s be worth so little that even IF the largest electronic prescription warehouses in the world came together to join hands it would be worth so little that the Federal Trade Commission would have to look into them for antitrust practices. Really they wouldn’t. After all it ain’t worth a dime, I mean, they say so:
The country's two largest electronic-prescription networks Tuesday announced a merger, creating a single, secure network for the exchange of digital health information.Gosh, I feel so much better knowing that this merger won’t be worth much to the companies, insurers, pharmacists, and drug company marketers and that the FTC can ignore this transaction! I mean, who needs competition, right? It’s all one big lovey-dovey moment! Can't you see those executives from the SureScripts-RxHub, LLC holding hands?
In a cashless transaction, which closed late Monday, RxHub LLC, a joint-venture of pharmacy-benefit managers, CVS Caremark Corp., Express Scripts, Inc. and Medco Health Solutions, Inc., will combine its operations with SureScripts, a private company founded by the National Community Pharmacists Association and the National Association of Chain Drug Stores. The merger isn't subject to antitrust review because the fair market value of the combined entity isn't high enough, according to the companies.
The owners of RxHub and SureScripts will each retain a 50% stake in the new venture, which will initially go by the name SureScripts-RxHub, LLC, according to executives from the two companies.
And why not? Their company won’t be worth much at all (really it won't), Congress will love it, AND they'll effectively have our healthcare system and privacy by the balls.
"Kum-ba-ya, my Lord. Kum-ba-ya..."
-Wes
Subscribe to:
Posts (Atom)